About Description
- reveals information about liver and kidney function
- determining diet and lifestyle affect health
Why People Choose Us

Quick & Easy
No appointment or long waiting times

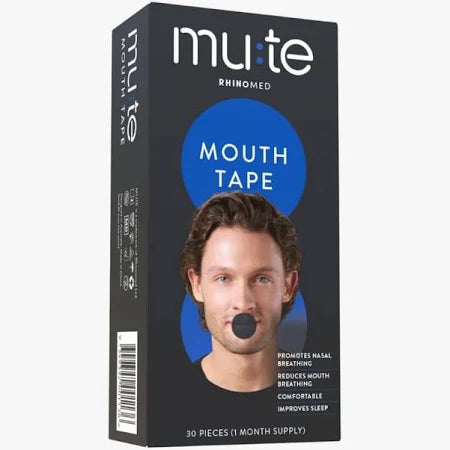
Discreet Packaging
Plain packaging with no medical stamps or marks

Confidential Service
Your information stays with us and private payment

UK Medication
Dispensed by registered UK pharmacists
Gout Risk (1 Biomarker)
Gout is a type of arthritis that usually affects the wrists, ankles, and joints in the fingers and toes. It results from an overabundance of uric acid building up and depositing crystals in the joints.
The big toe is frequently the target of the initial attack, which can be so painful and inflamed that the victim cannot bear to have anything touch it.
One or more joints may be affected by gout at the same time.
Steroids, non-steroidal anti-inflammatories, and colchicine are gout treatments.
Uric Acid
A byproduct of the breakdown of chemical molecules known as purines is uric acid. Purine is a substance that exists naturally in the body as well as in some meals more so than others.
Uric acid is normally eliminated by the kidneys in urine in healthy people, but if levels are too high or if you have a purine metabolism disorder, uric acid may start to build up and may deposit as crystals in the body tissues.
This results in the painful condition known as gout when it affects joints.
Liver Health (4 Biomarkers)
Muscle Health (1 Biomarker)
Creatine kinase
An essential enzyme in tissues with a rapid metabolism, such as muscle tissue, is creatine kinase (CK). One of the most noticeable by-products of the significant mechanical demands that sport and competitive training place on your body is CK, which seeps into the blood when your muscle fibers are worn out through repeated, powerful contractions.
Due to a number of processes, CK has historically been used in medicine as a marker indicating severe muscle damage.
High concentrations are potentially harmful and can build up to induce a terrible illness called "rhabdomyolysis." At this point, your body is breaking down so much muscle that the CK byproduct can make you ill and perhaps lead to kidney failure and a heart attack. An athlete's body, however, becomes adapted to handle far higher levels of CK than the normal person's body since muscle breakdown is essential to the anabolic process and occurs on purpose rather than accidentally.
Understanding normal CK levels is crucial because they might indicate whether a person can handle a higher training load or whether they need to cut back on their training. It is technically possible to raise your workload for faster, higher performance improvements, if you are a muscle-building athlete and your CK level, is below the normal range (from a CK perspective!).
Reduce your exercise load to avoid severe muscle damage, overtraining syndrome, and perhaps irreversible kidney damage if your CK level is too high. Always make sure to test your CK level at least two days after engaging in vigorous exercise to establish your baseline.
Cholesterol Status (6 Biomarkers)
Total Cholesterol
LDL cholesterol
Low density lipoprotein, often known as LDL cholesterol, is a lipid and protein molecule that carries triglycerides, cholesterol, and other fats to various bodily regions.
When fatty deposits build up inside artery walls due to an excess of LDL cholesterol, sometimes known as "bad cholesterol," this could result in atherosclerosis and heart disease.
Through food and exercise, your cholesterol levels can be dramatically reduced. Likewise, if you can raise your levels, you may be able to avoid developing significant, potentially fatal illnesses in the future.Results for HDL and LDL (and non-HDL) can be used as benchmarks and improvement targets. Regular exercise, especially cardio and weight training, will help lower LDL and raise HDL.
Cholesterol levels will also be optimised by a Mediterranean diet that is heavy in vegetables and oily fish and low in meat and dairy.
Non-HDL cholesterol
All of the cholesterol molecules that are not HDL (or "good" cholesterol") are referred to as non-HDL cholesterol. Therefore, it includes all of the potentially dangerous and non-protective cholesterol in your blood.
As a result, it is thought to be a more accurate indicator of cardiovascular risk than LDL cholesterol and total cholesterol. Less than 4 mmol/L of non-HDL cholesterol is advised. Through food and exercise, your cholesterol levels can be dramatically reduced. Likewise, if you can raise your levels, you may be able to avoid developing significant, potentially fatal illnesses in the future.
Results for HDL and LDL (and non-HDL) can be used as benchmarks and improvement targets.Regular exercise, especially cardio and weight training, will help lower LDL and raise HDL. Cholesterol levels will also be optimised by a Mediterranean diet that is heavy in vegetables and oily fish and low in meat and dairy.
HDL Cholesterol
High Density Lipoprotein, often known as HDL cholesterol, is a molecule that transfers cholesterol from the bloodstream to the liver, where it is broken down and expelled from the body as bile.
The term "good cholesterol" refers to HDL cholesterol. Through food and exercise, your cholesterol levels can be dramatically reduced. Likewise, if you can raise your levels, you may be able to avoid developing significant, potentially fatal illnesses in the future.
Results for HDL and LDL (and non-HDL) can be used as benchmarks and improvement targets. Regular exercise, especially cardio and weight training, will help lower LDL and raise HDL.
Cholesterol levels will also be optimised by a Mediterranean diet that is heavy in vegetables and oily fish and low in meat and dairy.
Total Cholesterol/HDL
By dividing your total cholesterol value by your HDL cholesterol level, you can get your cholesterol/HDL ratio. It serves as a gauge of cardiovascular risk since it provides useful information about the percentage of "good" cholesterol in your total cholesterol (i.e. high-density lipoprotein, HDL).
The cholesterol/HDL ratio is used by heart disease risk calculators (like QRisk) to estimate your risk of suffering a heart attack.
Triglycerides
Triglycerides are a type of lipid that move through the bloodstream. They are transported in the bloodstream by chylomicrons and VLDLs, two types of lipoproteins (very low density lipoproteins).
Following a meal, extra calories are converted by your body into triglycerides, which are subsequently carried to cells where they are stored as fat. Triglycerides are then released by your body when it needs energy.
Vitamins (3 Biomarkers)
Your body requires vitamins as necessary nutrients to function properly. They must come from the food you consume because you cannot manufacture them yourself. There are two categories of vitamins: fat-soluble and water-soluble.
Oily foods, whether animal- or plant-based, contain fat-soluble vitamins like vitamins A, D, E, and K.
You don't need to eat them every day because your body stores them in fatty tissue and the liver. You must consume meals containing these nutrients more regularly because the majority of water-based vitamins, such as vitamin C, are not stored in the body.
A balanced diet should provide you with all the vitamins you require. But occasionally, dietary decisions or medical issues might make us vitamin deficient.
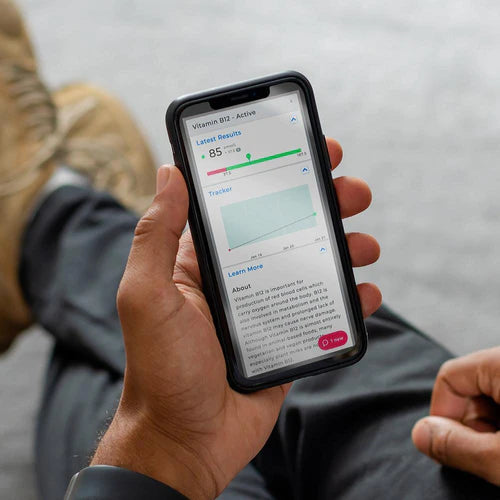
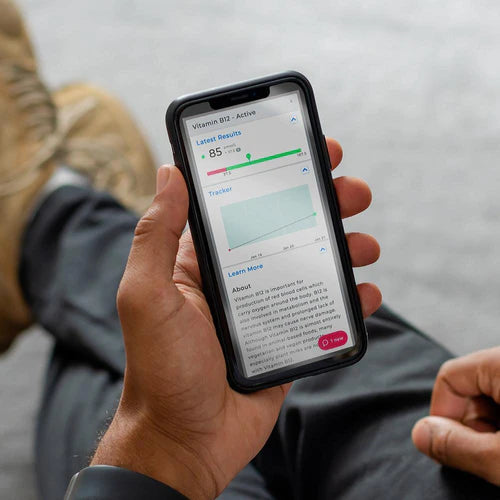
Vitamin B12
The generation of red blood cells, which transport oxygen throughout the body, depends on vitamin B12.
Additionally essential for metabolism and the nervous system, vitamin B12 deficiency can harm nerves over time.
Although plant milks are increasingly frequently enriched with vitamin B12, vitamin B12 is still nearly exclusively found in meals derived from animals.
Folate Serum
A coenzyme in the metabolism of amino acids is folate, a B vitamin. Additionally, it is necessary for the synthesis of purines and pyrimidines, which are necessary for the production of red blood cells and DNA.
Make sure your folate levels are normal if you're thinking about getting pregnant because folate is also crucial during the first trimester of pregnancy.
This vitamin helps athletes perform better by controlling energy metabolism by modifying the production and breakdown of carbohydrates, fats, proteins, and other bioactive molecules. It also works in conjunction with other B vitamins, such as vitamin B12.
Methylmalonic Acid Serum
Methylmalonic acid must be converted into coenzyme A by the action of vitamin B12. Methylmalonic acid will build up in the body rather than being converted to coenzyme A in vitamin B12 deficiency.
When B12 levels are near the lower end of the normal range, both active vitamin B12 and serum B12 levels can be normal in people who have the symptoms and biochemical signs of vitamin B12 deficiency.
Methylmalonic acid blood levels can be measured to determine if a B12 shortage is underlying.
Kidney Health (3 Biomarkers)
Waste materials and extra fluid are taken out of your blood by your kidneys. Examining the levels of waste products in the blood as well as the levels of electrolytes, which control fluid in the body, can be used to gauge how effectively they are performing their duties.
Early kidney disease signs are usually nonexistent, so it's crucial to keep an eye on kidney function, particularly if you have diabetes, high blood pressure, or a close relative who has the condition.
Creatinine
The regular breakdown of muscles produces the chemical waste molecule creatinine. Therefore, athletes are capable of higher levels than the normal person. Since creatinine is excreted by the kidneys, it can be used to diagnose renal disease and is a reliable indicator of kidney function.
Urea
When proteins are broken down in the liver, the body excretes urea as waste. After being created, urea is delivered to the kidneys, where it is removed from the blood and eliminated from the body as urine.
Thus, monitoring urea levels in the blood can provide insight into the health of the liver and kidneys. It is crucial to remember that findings may still come out as normal even if one kidney is seriously damaged but the other is in fine working order.
EGFR
The estimated glomerular filtration rate (eGFR), which calculates how much blood is filtered through the kidneys, measures how well the kidneys are functioning.
The kidneys' glomeruli are microscopic filters that remove waste materials. Kidney function may be hampered if these filters do not operate adequately.
Your age, gender, ethnicity, and serum creatinine levels are used to compute your estimated glomerular filtration rate, or eGFR.
Iron Status (4 Biomarkers)
Ferritin
A complex globular protein called ferritin is used to store iron in an inactive form. The ferritin releases its iron for usage as your iron reserves get depleted.
You will run out of iron if your ferritin levels drop, and your ability to make red blood cells in your bone marrow will also suffer.
Thus, ferritin provides a reliable indication of your iron reserves. Ferritin can rise at times of infection, inflammation, or trauma because it is an acute-phase protein as well.
Iron
Iron is essential for the activities that are essential for life, let alone athletic performance, such as oxygen transport, DNA synthesis, and oxidative phosphorylation. Red blood cells include oxygen-transporting haemoglobin, which contains roughly 2.1g, or about half of the body's total iron content.
A further gramme or so can be found in the oxygen-transporting myoglobin of muscles and in macrophages, which are white blood cells.
The liver is where extra iron is kept. You won't be able to breathe as efficiently at the cellular level if you have low iron levels, which will make you feel more exhausted and tyre more quickly.
This will affect athletes' performance, VO2 Max, energy efficiency, ability to train at their maximum capacity every day, maximum lactate level, and rate of exhaustion. Approximately 5% of your iron comes from food, and the remaining 95% comes from the breakdown and turnover of your red blood cells.
The two primary forms of iron in your diet are Fe2+, which is present in meat and dairy products, and Fe3+, which is more difficult to absorb and is present in plant-based foods.
Tests for iron status examine a variety of iron levels, which when combined can provide information about your iron metabolism and its implications for you.
TIBC
The total iron-binding capacity (TIBC) of your body is a gauge of how well it transports iron through the blood.
Transferrin Saturation
The primary blood protein that binds to iron and carries it throughout the body is called transferrin, which is produced in the liver.
This examination gauges the degree to which iron has "saturated" this protein.
Proteins (3 Biomarkers)
Proteins are essential for muscle growth as well as the operation of cells and tissues. Blood proteins are measured to assist in the diagnosis of various illnesses, such as liver or kidney disease.
It is common practise to analyse proteins to determine how much of a specific hormone is bound to a protein or free and thus available to your cells.
Proteins also transport other chemicals, such as hormones, throughout the blood. Dehydration is a common cause of elevated proteins, but they can also be a sign of other health issues.
A significant protein deficiency may be a sign of malnutrition or malabsorption.
Globulin
The term "globulin" refers to a variety of proteins that the liver and immune system create. While certain globulins transport metals like iron in the blood, others bind with haemoglobin.
In addition, there is a specific class of globulin called an immunoglobulin, which is another name for an antibody and aids in the body's defence against infection.
Albumin
A protein called albumin is mostly produced in the liver. It aids in generating the osmotic pressure necessary to keep water in the blood.
It is crucial for tissue growth and repair and aids in the transportation of nutrients, medicines, and other chemicals via the blood.
By evaluating albumin levels in the blood, we can determine how much hormone is available to your tissues. Albumin also transports hormones throughout the body.
Total Protein
The total protein in your blood is the sum of the proteins albumin and globulin. Among their many jobs, albumin and globulin keep blood in vessels, deliver nutrients, and combat infection.
A liver or renal problem as well as malnutrition may be indicated by abnormal levels.
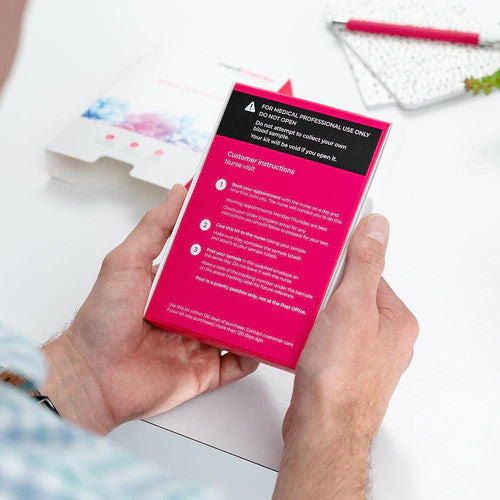
Easy Steps for your Medicine

Complete a consultation.
With complete privacy and confidentiality your form is checked by a pharmacist independent prescriber.
Choose your treatment.
From the list approved by the prescriber, choose your preferred treatment and then wait for it to be dispensed by UK Meds online pharmacy.
Receive your delivery
With next day delivery options available, you can have your treatment sent out to you discreetly within hours.Our Happy Customers
Rated Us for our Service Excellence
 Dispensed by Regulated UK Pharmacists
Dispensed by Regulated UK Pharmacists

 How it works
How it works Help
Help Account
Account
 Basket
Basket